Uptake
Founded Year
2014Stage
Incubator/Accelerator - II | AliveTotal Raised
$317MMosaic Score The Mosaic Score is an algorithm that measures the overall financial health and market potential of private companies.
-2 points in the past 30 days
About Uptake
Uptake specializes in industrial intelligence and predictive analytics within the software-as-a-service (SaaS) sector. The company offers solutions that translate data into insights for predictive maintenance, asset failure prediction, and optimization of maintenance strategies. Uptake primarily serves sectors that require maintenance analytics, such as transportation and heavy industry. It was founded in 2014 and is based in Chicago, Illinois.
Loading...
ESPs containing Uptake
The ESP matrix leverages data and analyst insight to identify and rank leading companies in a given technology landscape.
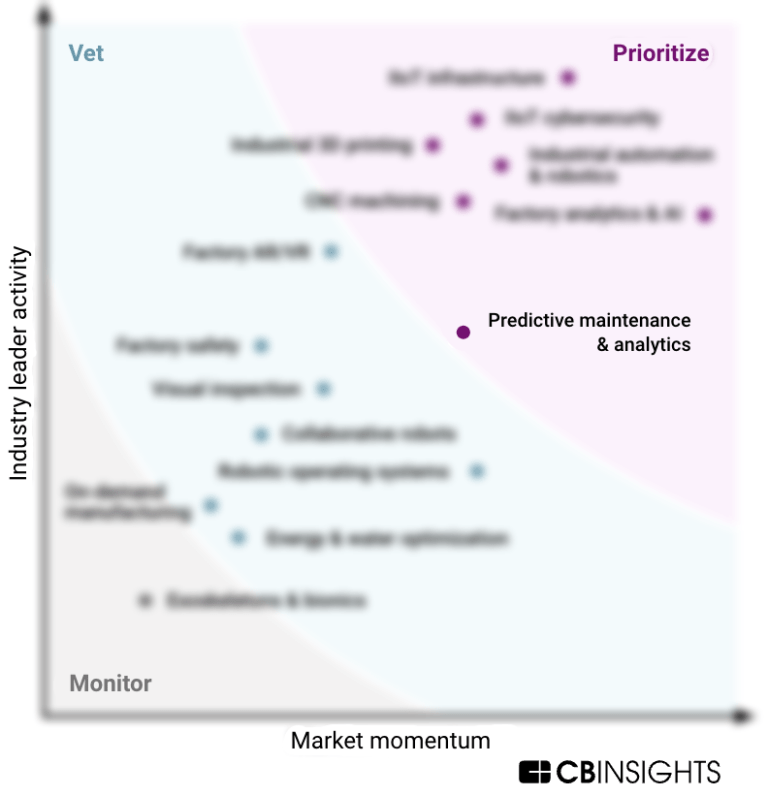
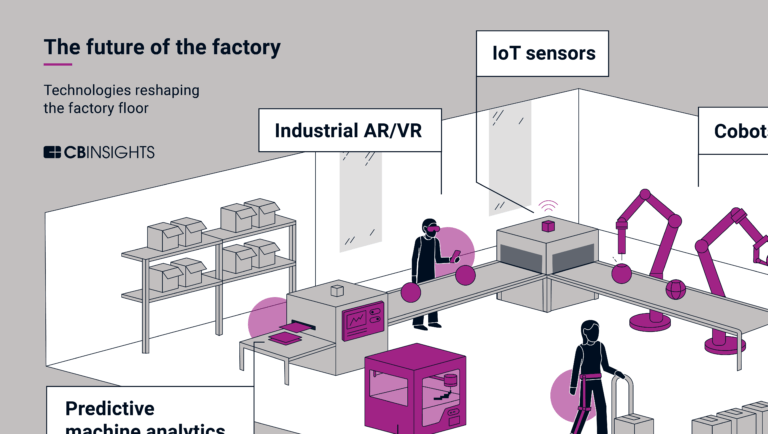
The predictive maintenance platforms market provides software solutions using AI and IoT technologies to provide real-time machine insights. This enables manufacturers to move from reactive to proactive maintenance programs, preventing process-driven production losses, reducing over-maintenance, extending asset lifetime, and optimizing manufacturing equipment controls. It also helps them eliminate…
Uptake named as Outperformer among 15 other companies, including IBM, Oracle, and Siemens.
Uptake's Products & Differentiators
Uptake Fusion
Uptake Fusion streamlines movement, storage, and curation of OT data, accelerating the transfer to the cloud while ensuring data integrity and security. The data is organized in the customer’s cloud environment on Microsoft Azure. Users across an organization, from multiple business units, have free rein to analyze the data, model the data, and customize it for a wide range of use cases that suit their specific needs.
Loading...
Research containing Uptake
Get data-driven expert analysis from the CB Insights Intelligence Unit.
CB Insights Intelligence Analysts have mentioned Uptake in 7 CB Insights research briefs, most recently on Mar 21, 2024.
Aug 16, 2023
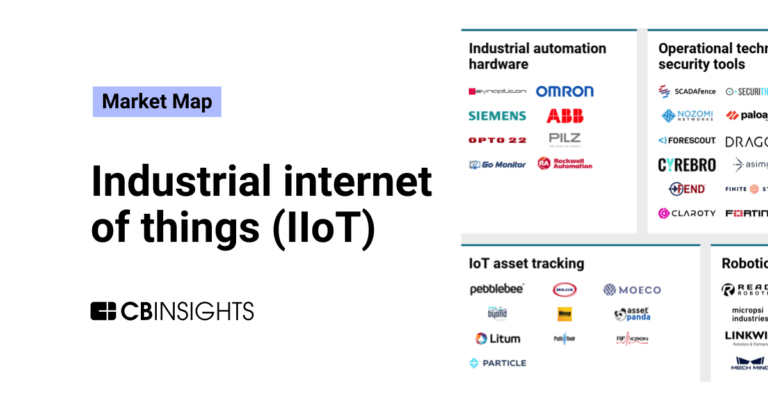
The industrial internet of things (IIoT) market map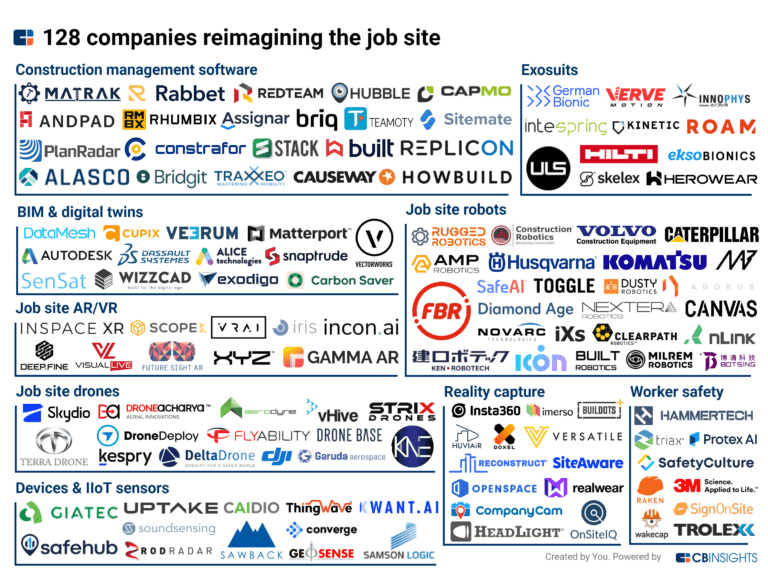
Nov 18, 2022
128 companies building the future of the job siteExpert Collections containing Uptake
Expert Collections are analyst-curated lists that highlight the companies you need to know in the most important technology spaces.
Uptake is included in 9 Expert Collections, including Construction Tech.
Construction Tech
1,460 items
Companies in the construction tech space, including additive manufacturing, construction management software, reality capture, autonomous heavy equipment, prefabricated buildings, and more
Supply Chain & Logistics Tech
4,273 items
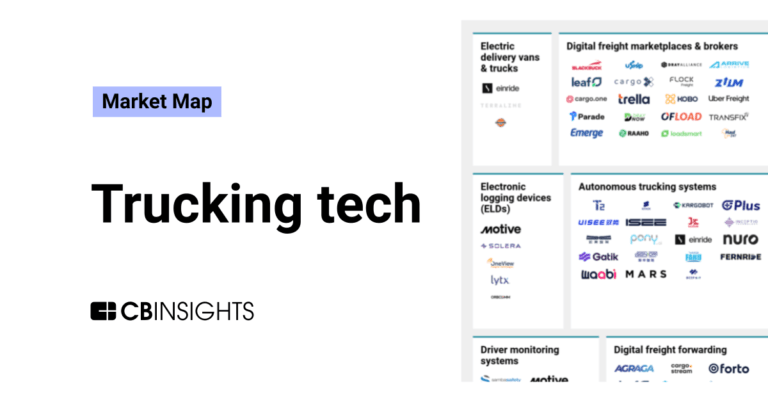
Companies offering technology-driven solutions that serve the supply chain & logistics space (e.g. shipping, inventory mgmt, last mile, trucking).
Unicorns- Billion Dollar Startups
1,261 items
Oil & Gas Tech
4,980 items
Companies in the Oil & Gas Tech space, including those focused on improving operations across upstream, midstream, and downstream sectors, as well as those working on sustainable fuels.
Tech IPO Pipeline
286 items
Energy Management Software
677 items
Companies creating software to help manage, optimize, and automate energy management and optimization.
Uptake Patents
Uptake has filed 89 patents.
The 3 most popular patent topics include:
- lung disorders
- respiratory therapy
- medical equipment
Application Date | Grant Date | Title | Related Topics | Status |
|---|---|---|---|---|
8/22/2022 | 11/5/2024 | Medical specialties, Seabird colonies, Autoimmune diseases, Rare diseases, Respiratory therapy | Grant |
Application Date | 8/22/2022 |
|---|---|
Grant Date | 11/5/2024 |
Title | |
Related Topics | Medical specialties, Seabird colonies, Autoimmune diseases, Rare diseases, Respiratory therapy |
Status | Grant |
Latest Uptake News
Dec 10, 2024
Victor Abiola Adepoju,1 Donald Chinazor Udah,2 Qorinah Estiningtyas Sakilah Adnani,3 Mohamed Mustaf Ahmed,4 Olalekan John Okesanya5 1Department of HIV and Infectious Diseases, Jhpiego (An Affiliate of Johns Hopkins University), Abuja, Nigeria; 2Department of TB Data, Impact Assessment and Communications Hub (TB DIAH), John Snow Research & Training Institute, Inc., Abuja, Nigeria; 3Department of Public Health, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia; 4Faculty of Medicine and Health Sciences, SIMAD University, Mogadishu, Somalia; 5Faculty of Medicine, Department of Public Health and Maritime Transport, University of Thessaly, Volos, Greece Correspondence: Mohamed Mustaf Ahmed, Email [email protected] Background: HIV self-testing (HIVST) offers a novel solution for increasing HIV testing among pregnant and postpartum women and their male partners, especially in low-resource settings. These groups often face barriers such as stigma, fear, and limited access to traditional HIV-testing services. Methods: We reviewed qualitative and quantitative studies focusing on HIVST implementation in both public and private healthcare settings among pregnant and postpartum women and male partners in sub-Saharan Africa (SSA), analyzed uptake, male involvement, and barriers. Articles from Scopus, PubMed, and Google Scholar were included to examine public and private settings, distribution models, and psychosocial support. Results: HIVST showed substantial success in increasing the testing rates. For example, maternal retesting during pregnancy has increased by 35% in Kenya due to the adoption of HIVST. The secondary distribution also drove male partner testing, with 90.8% of male partners accepting HIVST kits from their pregnant partners in South Africa and 75.4% participating in couple testing. Combining HIVST with clinical invitations increased both female and male testing 12-fold in other studies. Despite these successes, challenges persisted, with approximately 30% of women testing HIV-positive not returning to follow-up care. In addition, a few women reported adverse partner reactions, including intimate partner violence (IPV), after delivering HIVST kits. Conclusion: HIVST presents a critical opportunity to close gaps in HIV prevention between pregnant women and their male partners. Addressing barriers, such as stigma and enhancing male partner involvement, provides a pathway for more equitable testing practices. Scaling up successful community-based and secondary distribution models, alongside addressing challenges such as follow-up care and IPV concerns, is essential for reducing HIV transmission in SSA. Keywords: HIV self-testing, maternal retesting, male partner testing, intimate partner violence, linkage to care, HIV prevention, community-based distribution Introduction HIV self-testing (HIVST) has emerged as a transformative approach to global HIV prevention. The World Health Organization (WHO) recommends HIVST as an additional approach to improve HIV testing services. 1 As global health organizations strive toward the UNAIDS 95:95:95 goals, which aim to ensure that 95% of people living with HIV (PLHIV) know their status, HIVST offers a solution that increases accessibility and privacy, and institutionalizes behavioral changes towards frequent retesting among high-risk populations and those who have historically faced barriers to testing. 2–5 Pregnant and postpartum women, along with their male partners, represent a prioritized demographic due to their unique role in HIV prevention. Despite its potential, there is a critical gap in male partners’ engagement in HIV testing and care, particularly in SSA. This population group often faces additional barriers in traditional HIV testing settings, particularly in regions where conventional health services are difficult to access, including cultural stigma, a lack of male-friendly services, and limited awareness about the importance of testing. 6 Pregnant women attending antenatal care (ANC) and postpartum care are routinely tested as part of efforts to prevent mother-to-child transmission (PMTCT), making them a critical entry point for HIV intervention. However, male partners remain significantly poorly engaged in HIV testing and maternal care settings, a gap that impedes progress in achieving PMTCT goals. Addressing these gaps is essential for achieving broader HIV prevention goals in SSA. 7 This creates a significant gap in the prevention of HIV transmission between couples. Men generally have lower HIV testing rates, which increases the risk of HIV acquisition and transmission to their partners and children. 8 By encouraging mutual disclosure and fostering shared and discreet decision-making within households, HIVST could be game-changers in promoting couple-based HIV prevention strategies. Despite these advantages, challenges persist in the uptake and implementation of HIVST in SSA. These include questions about test accuracy, the ability of HIVST to address gaps in maternal retesting, particularly in low-resource settings, 9 and barriers to male-partner testing. 10 , 11 This review aims to examine the benefits, challenges, and opportunities HIVST offers pregnant and postpartum women and their partners in SSA countries, such as Kenya, South Africa, Uganda, Tanzania, and Nigeria, with a focus on testing uptake, autonomy, partner involvement, and improving maternal health outcomes, while providing a critical evaluation of the challenges and gaps that remain. Methods We conducted a literature review focusing on HIVST implementation among pregnant and postpartum women and their partners in SSA. We performed a literature search using Scopus, Google Scholar, and PubMed databases. The review includes both quantitative and qualitative studies to ensure a holistic approach to addressing HIVST in both public and private healthcare settings and to ensure comprehensive insights into implementation strategies and their broader applicability. We included only articles published in English, with no limitation of publication date relevant to the aim of addressing HIVST among the target population, and availability of data on key outcomes such as testing uptake, male partner involvement, and barriers and facilitators to care. Additional articles were identified by using the reference lists of the included studies. The selected articles were succinctly summarized under relevant headings owing to the limited scope of the study to analyze key metrics such as testing uptake, male partner involvement, and barriers and facilitators to care. The review included studies published both before and after HIVST became available in Africa. This approach allows for the incorporation of baseline insights into testing behaviors, barriers, and facilitators before the introduction of HIVST, and provides a more comprehensive understanding of how its implementation has influenced testing dynamics. Although we did not specifically track the number of articles sourced from each database (Scopus, Google Scholar, and PubMed), we ensured that the review was comprehensive by sourcing articles from widely recognized and reputable databases. This allowed for an inclusive search, and ensured that the selection of studies was based on relevance and quality rather than database-specific counts. The inclusion of multiple databases minimized the risk of publication bias and facilitated the inclusion of a diverse range of studies. This review examined the outcomes of different distribution models, including the secondary distribution of kits by women to their male partners, community-based delivery, and integration of psychosocial support. The inclusion of both public and private sector data is essential for informing conclusions and ensuring that recommendations are applicable to diverse healthcare contexts. Benefits of HIV Self-Testing for Pregnant and Postpartum Women Increased Autonomy and Agency One of the core benefits of HIVST is its ability to empower individuals, especially pregnant and postpartum women. HIVST provide them with greater control over their health in a private, non-stigmatizing setting. Traditional HIV testing in healthcare settings can be stigmatizing, and many women fear the public disclosure of their HIV status. HIVST provides private and confidential alternatives. HIVST enables these groups to take the test at the comfort of their homes. 12 This level of control promotes autonomy in testing and empowers women to discreetly manage their HIV status. Studies in SSA have shown that HIVST reduces anxiety and stigma, which are often associated with facility-based testing, encouraging more women to test early and frequently ( Table 1 ). 13 Table 1 Benefits, Challenges, and Strategies for HIV Self-Testing (HIVST) in Pregnant and Postpartum Women Increased HIV Testing Uptake Among Women The flexibility and accessibility of HIVST contributes to high HIV testing uptake among pregnant and postpartum women, particularly in low-resource settings. HIV testing during pregnancy is vital for PMTCT, and frequent re-testing during pregnancy, particularly in the third trimester, facilitates early detection of seroconversion ( Table 1 ). 14 In low-resource settings such as Sub-Saharan Africa (SSA), where access to healthcare may be sporadic, HIVST fills a critical gap by making testing accessible outside of clinical settings. For instance, in Kenya, studies have demonstrated that HIVST encourages retesting among male partners of women attending antenatal care, who may not otherwise attend healthcare facilities for follow-up testing. 8 Maternal Retesting During Pregnancy In SSA, where conventional HIV testing services (HTS) may be limited, and loss to follow-up is a concern, HIVST provides a valuable alternative for increasing access to testing. HIVST allows individuals to test outside of healthcare facilities, overcoming barriers like distance and stigma ( Table 1 ). 8 , 12 By offering HIVST kits during antenatal visits or through community health workers, health systems can ensure that women can retest at home. This ultimately reduces the risk of undiagnosed HIV infection and prevents vertical transmission to infants. Challenges in Using HIVST in ANC and Postpartum Settings False Negatives and Test Sensitivity/Specificity Although HIVST offers many advantages, one of its critical limitations is the potential for false negatives, particularly during pregnancy. Pregnant women experience physiological changes that can affect test accuracy. HIVST kits, although highly specific, fall short of 100% sensitivity, which can lead to false-negative results. 12 , 15 This poses significant risks for pregnant women, as an undiagnosed infection can lead to transmission to the fetus. Given this limitation, HIVST should be paired with routine facility-based testing in later stages of pregnancy, especially in settings where women are at a high risk of seroconversion ( Table 1 ). Challenges in Low-Resource Settings In low-resource settings, where the healthcare infrastructure is often weak, HIVST offers a practical solution for women who may struggle to access regular ANC services. 8 However, lack of proper follow-up mechanisms remains a significant challenge. Women who test positive for HIVST often face barriers in linking to care, particularly in rural areas, where healthcare facilities are distant and overburdened ( Table 1 ). 8 , 12 Furthermore, in these contexts, the risk of loss-to-follow-up (LFFU) is high because many women are unable to return to clinics for confirmatory testing or treatment after an initial positive result. HIVST for Male Partners of Pregnant and Postpartum Women Secondary Distribution by Women to Male Partners One of the most promising strategies to increase HIV testing among men is through the secondary distribution of HIVST kits by pregnant and postpartum women attending the ANC. 16 When women are given HIVST kits to take home, their male partners are more likely to test the privacy of their homes, free from the stigma or inconvenience of visiting a clinic. 16 The STAR Initiative in South Africa revealed that secondary distribution of HIVST kits through ANC clients and newly diagnosed individuals was highly effective and affordable. 17 Nearly all male partners accepted and used the kits, with significant proportions testing positive and linked to ART. 17 This approach included men who were otherwise difficult to engage in and facilitated high follow-up rates and treatment initiation. 17 This study underscores the strategic value of partner-delivered HIVST in scaling testing coverage, particularly in settings with access barriers, further reinforcing its role in improving HIV prevention outcomes. This method capitalizes on trust and communication between partners and offers men a non-confrontational way to test for HIV. Women often deliver kits at moments they perceive as emotionally opportune, and studies show that this approach leads to high rates of male partner testing. 18 In a study conducted in Malawi, both male and female participants found HIVST to be empowering. The authors further reported that mutual knowledge of each other’s HIV status cultivated openness and psychosocial support among partners, including support to adhere to ART and disclosure. 19 On the other hand, HIV-negative female sex workers in Kenya, whose partners tested positive, reported mixed reactions, including experiencing verbal abuse and terminating sexual relationships with the positive partner. 20 Similarly, a cluster-randomized trial reported that the sustained provision of multiple self-tests to women in Kenya led to an increase in male partner testing through secondary distribution. 21 However, despite this increase, the study did not find a significant reduction in HIV incidence between the intervention and control groups. This highlights the need for additional strategies to achieve the desired impact. Another study further supported these findings in a randomized trial in Kisumu, Kenya, where pregnant and postpartum women were provided with multiple self-test kits to distribute to their male partners. 16 The study demonstrated significantly higher rates of partner testing (90.8%) and couple testing (75.4%) in the HIVST group than in the clinic invitation group, without reports of intimate partner violence. 16 Increasing Male Partner Testing Male partner testing has historically created a significant gap in HIV prevention, particularly during pregnancy. Men tend to have lower rates of engagement with health systems because of societal norms, logistical challenges, and fear of a positive diagnosis. 8 HIVST offer an innovative way to address these barriers. Male partner testing rates have significantly increased in settings in which secondary distribution is used. 17 Successful strategies for engaging men include providing financial incentives, invitation letters, and leveraging peer support to encourage testing. 22 These efforts can substantially reduce the risk of vertical transmission and improve overall family health outcomes. However, HIVST has yielded mixed results in certain regions of SSA, with reports indicating a lack of consistent follow-up care and insufficient health system support in some areas, which has undermined its long-term effectiveness. 13 , 23 Challenges of Male Partner Involvement Despite these promising interventions, male involvement in HIV testing still presents considerable challenges. Many women initially felt anxious about how their male partners would react to receiving a HIVST kit at home. Despite their apprehension, most of them successfully delivered kits using various strategies. Some women strategically placed the kits in visible locations where their partners would naturally come across, prompting curiosity and encouraging discussion. 24 Many women also express concerns about intimate partner violence (IPV) or fear that their partners may react negatively to HIV testing. 17 In some regions, male involvement has been met with strong resistance, with many men expressing skepticism about the testing process and some perceiving it as a threat to their masculinity. This has led to challenges in scaling HIVST programmes. 22 A study examined stakeholder perceptions in Haiti regarding the secondary distribution of HIVST by women living with HIV (Option B+ patients) as a strategy to reach men. 25 Stakeholders expressed concerns about male partners’ reactions, limited support for self-testers, and potential risks of violence towards women. 25 This is particularly true in serodiscordant couples, where one partner is HIV-positive and the other is HIV-negative. However, they also highlighted the empowerment that HIVST provides and the autonomy to choose their preferred approach to testing, diagnosis, and treatment, particularly among the hard-to-reach groups. Ensuring that women receive supportive counselling before distributing HIVST kits is crucial for mitigating these risks. 25 Moreover, for male partners who test positive, lack of follow-up care remains a critical issue. Without proper post-test support, many men fail to seek confirmatory testing or treatment, leading to gaps in care. Delivery Models and Strategies for HIVST in ANC and Postpartum Care Home-Based vs Clinic-Based HIVST Home-based and clinic-based HIV self-testing (HIVST) models offer distinct advantages and challenges in antenatal care (ANC) and postpartum women. Home-based HIVST provide pregnant women and their male partners with the flexibility and privacy to test in their environments, free from the fear of stigma often encountered in clinics. 9 Studies have shown that home-based testing increases testing uptake, particularly among men who are usually reluctant to visit clinics. 8 Some women may feel more confident about receiving an HIV test from a trained healthcare professional, which can help address concerns about accuracy. The challenge with clinic-based models, particularly in low-resource settings, is the time and logistical burden that it places on individuals. Women and their partners must travel to clinics and often wait in long lines, which can discourage testing. Moreover, men frequently avoid clinic-based testing because of the stigma associated with being seen in a health facility, a space often perceived as feminine. 9 , 26 Therefore, while clinic-based HIVST provide better opportunities for immediate linkage to care, home-based models enhance autonomy and convenience, making it easier for individuals to test. Community and Peer-Based Distribution Models In community- and peer-based distribution models, community health workers or peers distribute HIVST kits. They targeted individuals in high-risk or hard-to-reach populations. These models have proven effective in scaling up HIV testing in low-resource settings, particularly by leveraging the existing community structures. 19 Community leaders or trusted peers act as mediators, reducing the stigma often associated with clinic-based testing. Community-based models have been shown to increase testing rates significantly, especially among individuals who may not seek testing on their own because of barriers such as transportation costs or stigma. For instance, in Malawi, HIVST distribution through community health workers has increased the number of people testing for HIV and improved early diagnosis. 27 , 28 By utilizing individuals who understand local contexts, these models facilitate better engagement and trust, making them ideal for low-resource or rural settings, where healthcare access is limited. However, scaling up these models presents challenges in terms of cost and sustainability. Community-based models rely heavily on trained personnel to distribute kits, provide counselling, and facilitate follow-up care. Maintaining a consistent supply of test kits and training sufficient community health workers remain a significant hurdle in resource-limited settings. To ensure the sustainability of community-based HIVST distribution, programs must integrate HIVST into broader health initiatives, such as maternal health or immunization programs, and explore cost-effective delivery options, such as mobile health platforms. 29 , 30 Linkage to Care and Post-Test Support for HIVST Linkage to Care Challenges The linkage to care remains one of the most critical challenges associated with HIVST, particularly in resource-limited settings. While HIVST increases testing rates, many individuals who receive a positive result fail to seek confirmatory testing or treatment because of logistical barriers, fear of stigma, or limited access to healthcare facilities. 31 In the context of pregnant and postpartum women, this poses significant risks not only to their health, but also to the health of their newborns. The lack of an immediate linkage to care undermines the potential of HIVST to prevent mother-to-child transmission. Innovative solutions such as peer navigation and mobile health (mHealth) interventions have shown promise in improving the linkage to care after HIVST. Peer navigation involves assigning trained individuals to guide newly diagnosed individuals through the healthcare system to facilitate confirmatory testing and linkage to care. 32 mHealth interventions, such as text message reminders or mobile apps, offer a cost-effective way to provide follow-up support and counselling, particularly in rural or low-resource settings. Despite these innovations, more work is needed to ensure that the linkage to care becomes a standard component of HIVST programs. Without reliable systems to connect individuals to care, the benefits of HIVST may be limited, especially for vulnerable populations, such as pregnant women and their male partners. 33 , 34 Post-Test Counselling and Emotional Support HIVST also highlights the need for post-test counselling and emotional support, especially for pregnant women, postpartum women, and their male partners. Receiving a positive HIV result can be an emotionally overwhelming experience, particularly without the immediate support of a healthcare professional. Many women, especially those living in serodiscordant relationships, fear the consequences of disclosing their status to their partners, which may include intimate partner violence (IPV) or abandonment. 9 , 35 To mitigate these risks, HIVST programs must incorporate robust counselling services. A study reported that HIV-positive women in Kenya reported that distributing HIVST kits to their male partners strengthened their relationships, improved condom use, and empowered them to make joint health decisions. 36 Importantly, the women did not experience intimate partner violence, which highlights the potential of HIVST to promote mutual support in serodiscordant couples when combined with proper counselling. Women who test positive require immediate access to professional support to navigate the complex emotional and social challenges associated with their diagnoses. In addition, male partners who test positive through HIVST should receive pre- and post-test counselling to ensure that they are adequately informed and supported throughout the testing process. Counselling delivered through in-person services or mHealth platforms can help individuals process their results and take the next steps in linking to care. 37 , 38 Acceptability and Willingness to Use HIVST Among Pregnant and Postpartum Women Factors Driving Acceptability Research has shown that HIVST is highly acceptable among pregnant and postpartum women. Acceptability is primarily driven by factors such as privacy, autonomy, and non-invasiveness. 39 A cross-sectional study in Nigeria revealed low HIV testing and counselling (HTC) uptake (35.8%) but a high willingness to self-test (70.4%). These findings highlight the feasibility of scaling HIVST in this context and setting. 40 For women who face stigma or fear of public disclosure of their HIV status, HIVST provides a confidential alternative that allows them to test in private. This level of autonomy is essential for women living in conservative or patriarchal societies, where independently accessing healthcare services can be challenging. Nevertheless, the ease of use and non-invasive nature of HIVST makes it appealing to women who are reluctant to undergo facility-based testing. The flexibility of being able to test at home at their convenience allows women to incorporate HIV testing into their routine without time constraints and logistical challenges associated with visiting a clinic. 21 , 41 Barriers to Uptake Despite its many advantages, several barriers limit HIVST uptake among pregnant and postpartum women. One of the primary concerns is the lack of post-test counselling.There is a low overall knowledge and utilization of HIVST among women in sub-Saharan Africa, with only 2.17% reporting awareness. 42 Factors such as age, educational level, wealth, and mass media exposure were associated with higher HIVST utilization. This study underscores the importance of targeted interventions that focus on addressing knowledge gaps and improving access to HIVST for women in rural and low-resource settings. Many women feel isolated after receiving a positive result from HIVST and are unsure of what steps to take next. Without immediate counselling or support, some women may delay seeking confirmatory testing or care, increasing the risk of HIV transmission to their infants. 43 Another barrier is fear of IPV. For many women, especially those in serodiscordant relationships, disclosing their HIV status to partners can trigger violence or abandonment. This fear often prevents women from distributing HIVST kits to their male partners or seeking follow-up care after testing. 44 , 45 Addressing this barrier requires tailored interventions that include safe counselling and confidential support services for at-risk women. Facilitators of HIVST Among Pregnant and Postpartum Women and Their Male Partners Several factors enhance the uptake and effectiveness of HIV self-testing (HIVST) among pregnant and postpartum women, and their male partners. User preferences play a significant role, with many preferring oral-based HIVST kits over blood-based ones due to their ease of use and non-invasiveness. Studies from Uganda have shown that couples prefer testing together, whereas others favor nurse-administered tests over self-testing. This emphasizes the need for flexible testing options. 18 Financial incentives have also been shown to boost participation, particularly among male partners, demonstrating that men are more likely to seek post-test services when financial incentives are offered along with HIVST kits delivered by their pregnant partners. 46 Similarly, a study in Kenya showed that distributing HIVST kits with invitation letters for clinic visits increased HIV testing. Raising awareness through mass media and SMS reminders has facilitated HIVST uptake. 26 A study reported improved testing outcomes among male partners in Kenya when SMS messages were used to encourage HIVST. 47 Moreover, combining interventions, such as distributing HIVST kits along with educational materials, pre-test counselling, and personalized invitation letters, have proven effective in maximizing male partner testing rates. 22 , 48 These facilitators highlight the importance of designing HIVST interventions that cater to user preferences, incorporate incentives, and leverage awareness campaigns to improve uptake and linkages to care. Adverse Outcomes of HIVST in Pregnant and Postpartum Women Risk of Intimate Partner Violence (IPV) The risk of intimate partner violence (IPV) has been cited as a potential adverse outcome of HIV self-testing (HIVST). The risk of IPV could be higher when women distribute self-test kits to their male partners, without disclosing their HIV status. Some studies indicate that women may fear their partners’ reactions to a positive result, which can lead to violence, emotional abuse, or abandonment. 49 , 50 A study found no significant adverse outcomes associated with HIVST. None of the women reported experiencing violence or adverse reactions after initiating discussions about HIVST with their partners. 18 This suggests that HIVST can be safely integrated into ANC settings with proper delivery and support. While there is concern about IPV, most studies have reported minimal adverse outcomes. A study found that partner distribution of HIVST kits sometimes led to temporary or non-resolving marital separations but no severe IPV incidents. 36 Similarly, a study conducted in Kenya examined the experiences of postpartum women and female sex workers with HIV self-testing. Although some women reported instances of IPV, these cases were isolated and no other adverse events were recorded. 21 These findings emphasize the importance of integrating pre- and post-test counselling into HIVST programs to mitigate such risks. 21 Emotional Impact and Psychological Stress Testing positive for HIV without immediate emotional support can leave pregnant women and their male partners psychologically vulnerable. The absence of professional counselling at the time of testing can increase stress, anxiety, and depression, especially when the test yields a positive result. 51 The authors reported that the lack of linkage to care after a reactive HIVST result could contribute to adverse emotional outcomes, including depression. This emotional toll is exacerbated by the isolation felt by individuals who test positive, particularly in the absence of mental health support. HIVST programs must prioritize mental health interventions in the overall care model. Providing emotional support is essential, whether through in-person counselling, mHealth interventions, or community-based support groups. By offering these services, HIVST programs can better equip individuals to manage the psychological and emotional challenges of receiving positive HIV results. 52 , 53 Moreover, integrating clear pathways to care and support for users will further reduce the risk of adverse outcomes associated with self-testing, which will promote safer and more effective public health interventions. 54 Conclusion and Future Directions HIVST offers significant potential to improve HIV testing among pregnant and postpartum women and their male partners. By providing privacy, autonomy, and convenience, it addresses many barriers associated with traditional facility-based testing. However, challenges remain, particularly in linking individuals to care after receiving positive results and providing adequate emotional support. To maximize its impact, this review recommends the development of actionable strategies for practitioners and policymakers. These include improving linkage-to-care systems to ensure timely treatment, enhancing the sensitivity and specificity of HIVST kits for antenatal and postnatal care, and integrating safe and accessible counselling services while addressing social and cultural barriers that limit uptake among pregnant women and their partners into HIVST programs. In addition, policy efforts must prioritize the provision of mental health support to address the emotional challenges often associated with HIV testing, while interventions must focus on reducing stigma and improving acceptance across different SSA regions. In conclusion, the integration of HIVST into maternal healthcare strategies, accompanied by robust support systems and community-based interventions, has the potential to significantly improve HIV prevention and care. This underscores the critical role of HIVST in achieving better health outcomes for both mothers and their partners in sub-Saharan Africa. Disclosure
Uptake Frequently Asked Questions (FAQ)
When was Uptake founded?
Uptake was founded in 2014.
Where is Uptake's headquarters?
Uptake's headquarters is located at 2045 West Grand Avenue, Chicago.
What is Uptake's latest funding round?
Uptake's latest funding round is Incubator/Accelerator - II.
How much did Uptake raise?
Uptake raised a total of $317M.
Who are the investors of Uptake?
Investors of Uptake include Plug and Play, GreatPoint Ventures, Revolution, Plug and Play Milan, Valor Equity Partners and 6 more.
Who are Uptake's competitors?
Competitors of Uptake include AspenTech, Amygda, Avathon, Coddi, Stimio and 7 more.
What products does Uptake offer?
Uptake's products include Uptake Fusion and 4 more.
Who are Uptake's customers?
Customers of Uptake include PepsiCo, Ensign Drilling and APS/Palo Verde Nuclear Generating Station.
Loading...
Compare Uptake to Competitors

Falkonry provides products that analyze operational data and enable condition-based actions related to reliability, quality, and sustainability. It serves the metals, defense and intelligence, chemicals, electronics and semiconductors, oil and gas, automotive, and pharmaceutical industries. It was founded in 2012 and is based in Cupertino, California. In August 2023, Falkonry was acquired by IFS.

Cognite offers an industrial software-as-a-service (SaaS) that specializes in digitalizing the industrial world. The company's main offering is Cognite Data Fusion (CDF), a software product that contextualizes operational technology (OT) and information technology (IT) data to develop scalable solutions for asset-intensive industries. Cognite primarily serves sectors such as oil and gas, power and utilities, renewable energy, and manufacturing, providing technologies that facilitate sustainable and efficient operations. It was founded in 2016 and is based in Lysaker, Norway.

Avathon specializes in artificial intelligence (AI) solutions across various sectors, including energy, manufacturing, government, education, and retail. The company offers products and services that enable predictive maintenance, fraud detection, and cybersecurity, with a focus on preventing zero-day attacks. Avathon's AI technology is designed to analyze and optimize data, augment human intelligence, and enhance operational efficiency. It was formerly known as SparkCognition. It was founded in 2013 and is based in Pleasanton, California.
DINGO is a global leader in Predictive Maintenance, providing software solutions for the Mining and Defence industries. The company offers enterprise-level software that predicts and prevents equipment failures, optimizes asset health, and aims to reduce maintenance costs while increasing production safety and efficiency. DINGO's software is used to manage the health of over $13.5 billion worth of heavy equipment, helping to save maintenance and replacement costs. It was founded in 1991 and is based in Wilston, Queensland.

Imubit specializes in AI process optimization for the hydrocarbon processing industry. The company offers a Closed Loop Neural Network Platform that leverages deep learning process control to enhance profitability, energy efficiency, and sustainability in refineries and chemical plants. It was founded in 2016 and is based in Houston, Texas.

Predictronics provides AI-based predictive analytics solutions within the industrial sector. The company offers services that include predictive maintenance, predictive quality, and condition-based maintenance, facilitated by their software platform, PDX. These services monitor critical assets, reduce unplanned downtime, and improve product quality for various industries. It is based in Cincinnati, Ohio.
Loading...