Cigna Healthcare
Founded Year
1982Market Cap
78.99BStock Price
283.99Revenue
$0000About Cigna Healthcare
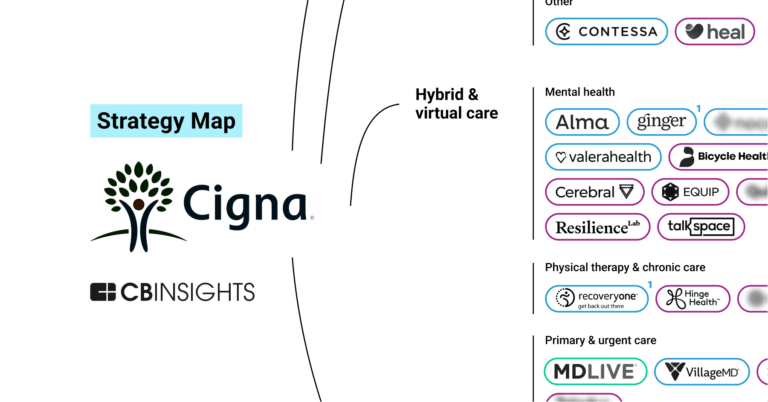
Cigna Healthcare provides health benefits through various health insurance plans for individuals, families, and employers. The company offers products such as medical, dental, supplemental health insurance, and Medicare coverage, primarily serving the healthcare and insurance sectors. It was founded in 1982 and is based in Bloomfield, Connecticut.
Loading...
Loading...
Research containing Cigna Healthcare
Get data-driven expert analysis from the CB Insights Intelligence Unit.
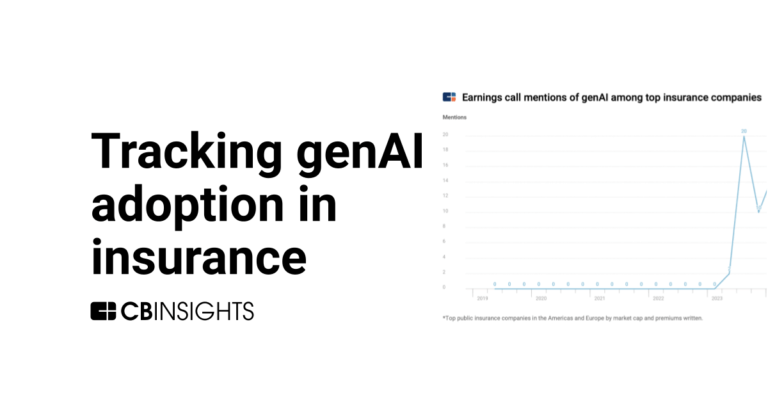
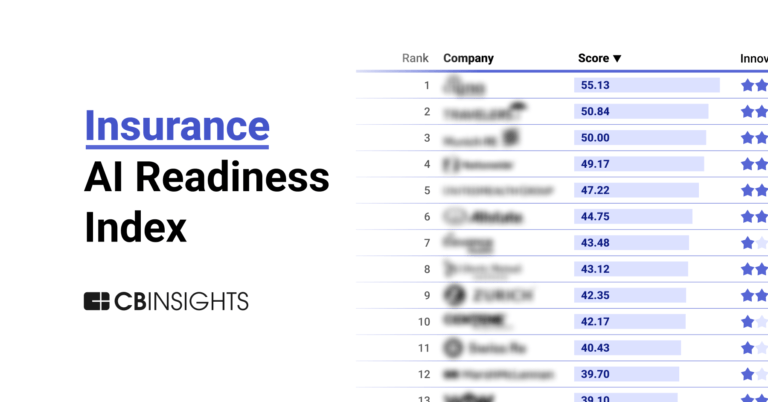
CB Insights Intelligence Analysts have mentioned Cigna Healthcare in 6 CB Insights research briefs, most recently on Jul 19, 2024.
Expert Collections containing Cigna Healthcare
Expert Collections are analyst-curated lists that highlight the companies you need to know in the most important technology spaces.
Cigna Healthcare is included in 1 Expert Collection, including Fortune 500 Investor list.
Fortune 500 Investor list
590 items
This is a collection of investors named in the 2019 Fortune 500 list of companies. All CB Insights profiles for active investment arms of a Fortune 500 company are included.
Cigna Healthcare Patents
Cigna Healthcare has filed 78 patents.
The 3 most popular patent topics include:
- data management
- machine learning
- computer network security
Application Date | Grant Date | Title | Related Topics | Status |
|---|---|---|---|---|
7/20/2023 | 10/15/2024 | Machine learning, Numerical climate and weather models, Statistical forecasting, Regression analysis, Meteorological data and networks | Grant |
Application Date | 7/20/2023 |
|---|---|
Grant Date | 10/15/2024 |
Title | |
Related Topics | Machine learning, Numerical climate and weather models, Statistical forecasting, Regression analysis, Meteorological data and networks |
Status | Grant |
Latest Cigna Healthcare News
Jan 16, 2025
UnitedHealth’s annual net income plummeted to $14.4 billion — its smallest since 2019 — as the company spent billions to recover from a cyberattack. Published Jan. 16, 2025 Listen to the article 8 min This audio is auto-generated. Please let us know if you have feedback . UnitedHealth brought in a record $400.3 billion in revenue in 2024 despite a string of crises for the nation’s largest healthcare company, including a massive cyberattack, heavy congressional and regulatory scrutiny and the shooting of its top insurance executive. However, UnitedHealth’s annual net income plummeted to $14.4 billion — its smallest profit since 2019 — as the company spent billions to recover from the cyberattack on claims processing subsidiary Change Healthcare and made less from offering Medicare and Medicaid plans, according to financial results released Thursday morning. Still, when excluding the cyberattack costs (and other factors UnitedHealth believes aren’t representative of its overall business performance in the year), the Minnesota healthcare behemoth reported adjusted profit of $25.7 billion — an all-time record. Without Change and other factors, UnitedHealth reported record profit last year UnitedHealth’s unadjusted and adjusted net income, 2014-2024 In a call with investors Thursday morning, executives acknowledged widespread discontent with the U.S. healthcare industry in their first public comments since UnitedHealthcare CEO Brian Thompson was killed in December . During the call, CEO Andrew Witty argued the firestorm was indicative of larger problems with the healthcare system — not just health insurers — and placed blame on hospitals for overbilling for care and on drugmakers for setting high list prices for medications. “Fundamentally, healthcare costs more in the U.S. because the price of a single procedure, visit or prescription is higher here than it is in other countries. The core fact is that price, more than utilization, drives system costs higher,” Witty said. Still, the CEO pledged that UnitedHealth will work this year to improve the speed and accuracy of claims processing, reduce processes that can slow down procedure approvals and better communicate with its members. “If you look at the mission of the company, it’s all about trying to improve the health system for everybody,” Witty said. “We recognize there’s still a lot of work to be done in that regard.” Optum Rx pledges 100% rebate pass-through Criticism of UnitedHealth’s business practices has also hit its pharmacy benefit manager, Optum Rx. The company is one of the so-called “Big Three” PBMs, along with Cigna’s Express Scripts and CVS’ Caremark, which jointly account for about 80% of U.S. prescriptions. Lawmakers on the Hill have proposed a number of bills targeting how PBMs do business in a bid to lower drug prices. And earlier this week, the Federal Trade Commission — which is suing all three companies — released its latest report on the industry that accuses the Big Three of jacking up the prices of specialty drugs. Amid Washington’s focus on PBM reform, Optum Rx plans to phase out all models that allow it to retain savings from negotiations with drugmakers over the next three years, Witty said. The CEO noted that Optum Rx already passes through 98% of rebate discounts, but the remaining fraction it retains gives critics leverage to argue PBMs are profiteering from their middleman status in the drug supply chain. “We’re committed to fading out those remaining arrangements so that 100% of rebates will go to customers by 2028 at the latest,” Witty said. “This will help make more transparent who is really responsible for drug pricing in this country: the drug companies themselves.” UnitedHealthcare’s underwhelming results UnitedHealth has also been dealing with a more quotidian issue with offering health insurance: errors in predicting the cost of medical care its members used last year. These problems dragged into the fourth quarter, with the company recording a medical loss ratio of 87.6%, well above analyst expectations. Specifically, the Biden administration’s changes to how health insurers code members’ risk in Medicare Advantage have lowered reimbursement, even as seniors use more medical care than insurers planned. And in Medicaid, states’ payment rates continued to land below the cost of caring for beneficiaries in the safety-net program in the fourth quarter, CFO John Rex said. Higher hospital coding intensity and specialty medication prescribing also drove up medical costs in the quarter. The underwhelming results are a bad sign for the rest of the earnings season, which UnitedHealth kicks off each year. Other publicly traded insurers are likely to report similar expense pressures, causing stocks in Humana, CVS, Elevance, Centene and Cigna to dip in premarket trading Thursday. UnitedHealth’s financial outlook for 2025 projects further increases in medical costs, with an expected MLR of 86.5% at the midpoint, up from the 85.5% lodged this year. However, executives stressed that UnitedHealthcare plans for 2025 are well-situated to absorb any continuing pressures. States continue to increase their Medicaid rates. And MA enrollment during the signup period in the fall was strong, Rex said. That includes a tickup in seniors electing for more managed care options like HMOs, plan designs that limit coverage to specific providers, that result in more predictable spending for the insurer, according to the CFO. “We feel very good about how we priced into [2025]. We feel really, really good about how the mix is coming in terms of that growth. That’s a huge difference from [2024],” Witty said. UnitedHealthcare expects to add about 800,000 MA members this year. The insurer closed 2024 with 50.7 million medical members overall. Final Change bill: $3.1B In one of the greatest hits to its bottom line last year, UnitedHealth’s Change Healthcare was struck with a ransomware attack in February that breached the data of 100 million people and took its systems offline for months, causing a cascade of billing problems for providers nationwide. Final cyberattack costs of $3.1 billion in 2024 blew past initial spending estimates. UnitedHealth initially expected $1.6 billion in costs, before revising the outlook to $2.9 billion in October. The attack also reignited anticompetitive concerns about UnitedHealth’s 2022 acquisition of Change . The $13 billion deal was opposed by regulators in the Department of Justice who argued it would give UnitedHealth access to vast amounts of data from its health insurance rivals and unprecedented market power in the claims management space. Still, a judge allowed the deal to go through. UnitedHealth reaffirmed its 2025 outlook following the fourth-quarter results, including revenues of $450 billion to $455 billion this year. Recommended Reading
Cigna Healthcare Frequently Asked Questions (FAQ)
When was Cigna Healthcare founded?
Cigna Healthcare was founded in 1982.
Where is Cigna Healthcare's headquarters?
Cigna Healthcare's headquarters is located at 900 Cottage Grove Road, Bloomfield.
Who are Cigna Healthcare's competitors?
Competitors of Cigna Healthcare include NeueHealth, Intermountain Health, Truveris, Advocate Aurora Health, Excela Health and 7 more.
Loading...
Compare Cigna Healthcare to Competitors
Alignment Health operates as a health insurance provider focused on offering Medicare plans. The company provides on-demand access to healthcare services, including in-person, in-home, and mobile device consultations, along with a range of all-inclusive benefits for its members. The company primarily serves the Medicare beneficiaries sector. It was founded in 2013 and is based in Orange, California.

Blue Cross Blue Shield is a federation of independent health insurance companies that offer health care insurance for individuals, families, and employers, along with Medicare plans. It was founded in 1910 and is based in Chicago, Illinois.

Endeavor Health is a healthcare system operating in the health services sector. The company provides medical services including emergency care, immediate care, walk-in clinics, and health risk assessments, along with a patient portal for managing health online. Endeavor Health was formerly known as Edward-Elmhurst Health. It was founded in 1995 and is based in Evanston, Illinois. In January 2022, Endeavor Health merged with NorthShore University HealthSystem.

RxBenefits is a pharmacy benefits optimizer. It operates within the healthcare and pharmaceutical industries. The company specializes in providing pharmacy benefit solutions, leveraging purchasing power, independent clinical solutions, and services to manage drug costs for employer-sponsored medical plans. RxBenefits primarily serves benefits advisors, employers, healthcare markets, labor and trust organizations, private equity firms, and third-party administrators. It was founded in 1995 and is based in Birmingham, Alabama.

Flipt is a healthcare technology and services company that specializes in pharmacy benefit management within the healthcare sector. The company provides a software platform that integrates benefits administration, formulary development, prior authorization, pharmacy network management, claims adjudication, and member services for pharmacy benefits management. It is based in Jersey City, New Jersey.

Blue Cross and Blue Shield of North Carolina is a health insurance provider offering individual and family health insurance plans, Medicare, dental, and vision options, as well as plans for small and large employers. It was founded in 1933 and is based in Durham, North Carolina.
Loading...